David Bell (University of Stirling), Adelina Comas-Herrera (Care Policy and Evaluation Centre, London School of Economics and Political Science) , David Henderson (Edinburgh Napier University, Scottish Centre for Administrative Data Research), Siôn Jones (LE Wales and London Economics) Elizabeth Lemmon (University of Edinburgh, Edinburgh Health Economics), Mirko Moro (University of Stirling), Siobhán Murphy (Centre for Public Health, Queens University Belfast), Dermot O’Reilly (Centre for Public Health, Queens University Belfast), Pietro Patrignani (LE Wales and London Economics)
The full report is available here:
Summary
The impact of the COVID-19 pandemic on the oldest old, especially those within care home settings, has been devastating in many countries. The UK was no exception. This article reviews the path of the COVID-19 pandemic across the UK long-term care (LTC) sector, indicating how it evolved in each of the four home nations. It prefaces this with a description of LTC across the UK, its history and the difficulties encountered in establishing a satisfactory policy for the care of frail older people across the home nations.
The paper makes several contributions. First, it provides an up to date estimate of the size of the adult care home sector across the UK – previous work has been bedevilled by inaccurate estimates of the number of care home places available. It also assembles the limited information that is available on delayed transfers of care and testing of care home residents, both of which played a role in the evolution and consequences of the pandemic. Its most important contributions are estimates of the number and share (the P-Score) of “excess deaths” in care homes in each of the home nations. The P-Scores provide measures that allow comparisons across care home populations of different size. Not only do we discuss the number of individuals affected, we also compare the proportions of care homes in each of the home nations that experienced a COVID-19 infection. The paper also discusses deaths of care home residents outside care homes, largely in hospitals. It reviews the sparse information on deaths at home of people who were receiving social care.
Throughout our narrative, it will become clear that there have been major deficiencies in both the amount and the consistency of data available to clinicians, care sector staff and researchers trying to understand and to alleviate what has happened in care homes. Thus, the final section makes some recommendations about the scope and timeliness of relevant data. Collection of such data would seem to be a necessary condition to inform best practice and thus avoid a repeat of the troubling effects of the pandemic on people who use formal care between March and June 2020.
Main findings:
Size of the UK care home sector
To correct widespread misreporting of the size of the UK care home sector, we collected information from each of the four home nation care regulators. This gave us estimates of the number of care homes and allowed us to estimate the number of care home residents.
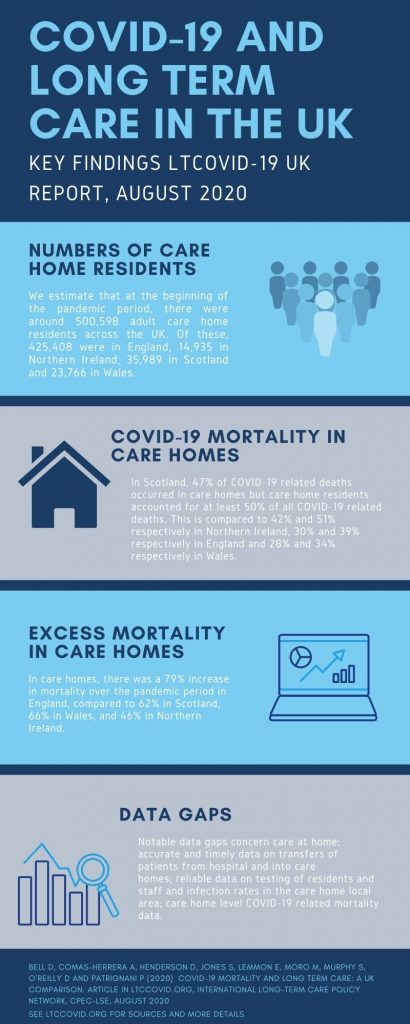
- In total, there are 18,075 care homes for adults across the UK. The most recent regulatory reports show 15,481 care homes in England, 481 in Northern Ireland, 1,057 in Scotland and 1,056 in Wales. We estimate that at the beginning of the pandemic period, there were around 500,598 adult care home residents across the UK. Of these, 425,408 were in England, 14,935 in Northern Ireland, 35,989 in Scotland and 23,766 in Wales.[1]
- There are significant differences in the numbers of care home residents per thousand adults and per thousand older populations across the home nations. These reflect differences in the demography and prevalence of disability at different ages. They also reflect policy differences around the “balance of care” – the extent to which policy is supportive of care home provision relative to domiciliary care or other accommodation solutions.
UK COVID-19 related deaths of care home residents
Across the UK, COVID-19 mortality data are broadly comparable. All four nations use the emergency ICD-10 codes for recording COVID-19 related deaths and publish these data weekly on their respective statistical authority websites. Some, but not all, of these reports provide a breakdown of deaths by location of death (care home, hospital and other), both current and historic. Nevertheless, we were able to assemble comparable data on deaths in care homes for each of the home nations and on the number and share of care homes where an infection took place. We also collected some limited data on deaths of care home residents outside care homes.
- We define the pandemic period from the registration of the first COVID-19 related death during week 11 (ending 13th March) in England up until week 26 (ending 26th June). There are slight differences in the recording of weeks by the nations and it is important to note that each country may have entered the pandemic at different times, and this may affect estimates of excess deaths and P-Scores.
- Throughout this period, 54,510 COVID-19 related deaths were registered in the UK, across all age groups and all locations of death. There were significant differences in COVID-19 related deaths per 100,000 individuals across the UK. These were highest in England, at 84 deaths per 100,000. Northern Ireland’s were lowest at 44 per 100,000. In Wales and Scotland, by week 26, deaths per 100,000 individuals stood at 77 and 76 respectively.
- Of all deaths registered as COVID-19 related in the UK, 17,127 (31%) occurred within care homes and at least 21,775 (40%) were accounted for by care home residents. There were differences across the UK. In Scotland, 47% of deaths attributed to COVID-19 occurred in care homes. This compares with 42% in Northern Ireland, 30% in England and 28% in Wales. In terms of deaths accounted for by care home residents, once again there are differences between the home nations. In Northern Ireland, care home residents accounted for 51% of all COVID-19 related deaths, compared to 50% in Scotland, 50%, 39% in England and 34% in Wales.
- Data on the share of care homes reporting at least one case of suspected or confirmed COVID-19 in Scotland show that 65% of all care homes reported cases. This is compared to 44% of all adult care homes in England, 37% in Northern Ireland and 33% in Wales reporting confirmed or suspected COVID-19 cases. It appears that Scotland had the largest share of affected care homes, though some care must be taken with this conclusion given that it is not clear that all of the home nations use the same definition of an outbreak.
Excess deaths during the pandemic period
Excess deaths are those deaths in excess of some measure of average or normal deaths over some comparable historic period. For deaths in care homes, we used average weekly deaths during the previous 5-year period. The absolute numbers of excess deaths were transformed to P-Scores by expressing excess deaths as the percentage increase over average historic deaths. This allows meaningful comparison between areas that differ substantially by size of population and record COVID-19 related deaths in different ways.
- Using this measure, we find that over our defined pandemic period England had a 38% increase in mortality compared with 29% in Scotland, 22% in Wales, and 20% in Northern Ireland. Breaking this figure down by location of death reveals a 79% increase in mortality over the pandemic period in English care homes compared to 62% in Scotland, 66% in Wales, and 46% in Northern Ireland. Thus, although Scotland had the highest proportion of care homes infected and the highest proportion of deaths attributed to COVID-19 in care homes, it had a lower proportion of excess deaths in care homes than in England or Wales. This may reflect differences in testing practices and death registrations across the nations. Northern Ireland had both the lowest share of care homes infected and the lowest level of excess deaths in care homes.
- Given that, due to the variation in testing procedures and recording of deaths, it will never be possible to unequivocally assign care home deaths during the pandemic to COVID-19 or other causes, the judgement on relative failure or success in handling the pandemic in care homes must ultimately rest with comparative performance in relation to excess deaths. This internationally recognised approach deals both with misdiagnosed deaths and also deaths that have other immediate causes, but which would not have occurred in the absence of the pandemic. By this measure, Scotland, Wales, and particularly England appear to have performed poorly.
Relative impact of the COVID-19 pandemic on the care home population
As the share of adults living in care homes varies between the four nations, comparing the number of deaths of care home residents registered as involving COVID-19 and of excess deaths to the numbers of people living in care homes can show the relative impact of the COVID-19 pandemic among the care home population in the four nations.
- We find that, in terms of deaths registered as involving COVID-19, during our defined pandemic period, deaths of care home residents in the UK represented just over 4% of all care home beds (ranging from 2.6% in Northern Ireland to 5.4% in Scotland). In terms of excess deaths in care homes (and, due to lack of historical data, not including deaths of care home residents in hospital), these represented nearly 5.5% of care home beds in the UK. The share of residents who died would be higher.
Testing strategy in UK care homes
The testing strategy has been characterised by dramatic changes and has followed a similar pattern across all the four nations. Initially, testing was limited to a few residents with symptoms. The focus moved towards testing people discharged from hospitals to care homes and symptomatic staff in mid-April. More recently testing guidelines have been recognising the role played by asymptomatic transmission by both residents and staff. The four nations are all currently committed to regular testing and retesting collected on site. Doubts remain about the implementation of this ambitious strategy, given reports of limited testing capacity and data gaps across the four nations. Alternative approaches based on the rate of infection in the local area and adoption of innovative strategies such as pool testing and saliva-based testing kits should be considered.
Mortality among people using care at home
England is the only UK nation that has released COVID-19 mortality data on those receiving care at home. That data show that throughout the pandemic period there were a large number of excess deaths in the domiciliary setting. The majority of which were not recorded as being COVID-19 related. Overall, the English data demonstrate that, compared to care homes, the overall proportional increase in deaths was greater in the domiciliary setting[2].
Data limitations
Several data gaps limit our ability to offer a full account of the impact of COVID-19 within the LTC system. Most notable are the gaps surrounding care at home including data on unpaid carers and individuals’ choices over purchasing care; accurate and timely data on transfers of patients from hospital and into care homes; reliable data on testing of residents and staff and infection rates in the care home local area; care home level COVID-19 related mortality data.
Going forward, the urgency of the need to invest more resources into the collection of social care data and statistics has never been more apparent. Acting on the key messages and recommendations set out by the Office for Statistical Regulation (OSR) in their reports into adult social care statistics provides a starting point to prepare and ensure the devastating impact of COVID-19 in the care sector is not repeated.
About this report:
We attempt to present comparable data and statistics on the effect of COVID-19 within long-term care (LTC) settings in the UK, with a particular focus on care homes. We begin in Section 1 by providing a background to LTC policy and provision in the UK. In Section 2 we outline the ways each of the UK nations records COVID-19 mortality and the data sources for each. Further, we highlight the additional sources of mortality data on care home residents that are comparable across the four nations. These data sources inform our analysis in the subsequent sections. In Section 3, we describe the path of the pandemic throughout the UK, presenting data on COVID-19 mortality and the impact of COVID-19 within care homes. In Section 4, we present data on excess mortality – as one of the key metrics to assess the mortality impact of the pandemic and to make robust comparisons between countries – across the UK and by location of death. Section 5 highlights the testing regimes and their evolution. Section 6 comments on the impact of COVID-19 within the care at home setting. Finally, Section 7 discusses the findings and concludes.
The code for the figures in the report is available here
[1] See Table 1 for sources.
[2] Hodgson et al, 2020. Briefing: Adult social care and COVID-19 Assessing the impact on social care users and staff in England so far. Available here.
Please cite as:
Bell D, Comas-Herrera A, Henderson D, Jones S, Lemmon E, Moro M, Murphy S, O’Reilly D and Patrignani P (2020) COVID-19 mortality and long term care: a UK comparison. Article in LTCcovid.org, International Long-Term Care Policy Network, CPEC-LSE, August 2020

Spotted a typo in the summary. “The focus moved towards testing people discharged from to care homes and symptomatic staff in mid-April.”
*hospitals*?
Thank you, will correct ASAP!
A good report – but the biggest gap in the data is the effects of six months isolation from relatives and friends and believe me it’s not getting any better, Prison style thirty minute visits outside once a week or once a fortnight are no way to rebuild relationships with loved ones who have been isolated and abandoned.
Thank you, this report focuses on mortality data, but there are other reports on the website (and more in preparation) addressing the impact of isolation, it is a really important issue indeed and we are keeping a close eye on emerging evidence and seeking to share examples of good practice
Some posts/reports on this so far:
https://ltccovid.org/2020/07/01/detrimental-effects-of-confinement-and-isolation-on-the-cognitive-and-psychological-health-of-people-living-with-dementia-during-covid-19-emerging-evidence/
https://ltccovid.org/2020/07/10/national-and-regional-guidance-relating-to-allowing-family-and-other-visitors-back-into-care-homes/
https://ltccovid.org/2020/07/19/finding-the-right-balance-an-evidence-informed-guidance-document-to-support-the-re-opening-of-canadian-long-term-care-homes-to-family-caregivers-and-visitors-during-the-covid-19-pandemic/
Great stuff, congrats to the authors. A really useful report. A most reassuring sentence is: “Given that, due to the variation in testing procedures and recording of deaths, it will never be possible to unequivocally assign [care home] deaths during the pandemic to COVID-19 or other causes, the judgement on relative failure or success in handling the pandemic [in care homes] must ultimately rest with comparative performance in relation to excess deaths.” My square brackets show that, if you omit the references to care homes, the same applies to the general population. That stark reality is relevant to all the speculation about the performance of different jurisdictions in response to Covid.
Really interesting report – there is just one area that seems to be missing and that is what the impact is on working age disabled people, particular of interest is people with learning disabilities, many of whom will use supported living arrangements (in fact this is actively preferred by many commissioners in England to the care home model, and of course people with learning disabilities themselves). The focus on older people’s homes has unfortunately led to these arrangements suffering when it comes to prioritising testing and other support from government, and asymptomatic ‘whole service’ testing is still not available for those in supported living in England and whole home testing was only extended to the ‘under 65s’ in care homes many weeks after the care home testing announcement. This is despite the known risks to people with learning disabilities from Covid and the health inequalities people already experience, as well as discrimination (see blanket DNRs also being applied to people in these settings).