Adelina Comas-Herrera, Joseba Zalakaín, Charles Litwin, Amy T. Hsu, Natasha Lane and Jose-Luis Fernández
The international report on the number of deaths in care homes linked to the COVID-19 pandemic has now been updated and is available here:
Since the first version of this report of the 12th of April, an increasing number of countries are publishing data on deaths of care home residents (or deaths in care homes) linked to COVID-19, the authors are very grateful to all who have provided information about data availability in their countries.
There continues to be a lot of differences in how the data is collected and what it covers. The key differences are due to whether the data covers deaths of care home residents (irrespective of whether they die in the care home or hospital) or just deaths that happen in the care homes. Another important difference is whether the deaths reported (both among care home residents and the whole population) cover cases confirmed through testing, cases where COVID was considered to be the probable cause of death, or excess mortality during the period of the pandemic.
For England we have data from the Office for National Statistics on probable COVID-19 deaths of people who died in care homes and excess deaths, both for people who died in care homes and of care home residents. This provides a good example of why it is important to ensure that we have, as much as possible, similar approaches to reporting deaths of care home residents: in England the share of all probable COVID-19 deaths in care homes is 27%, the share of all probable COVID-19 deaths of care home residents is 38%. The share of excess deaths in care homes is 44% and the share of deaths of care home residents is 52% of all excess deaths. Also, in France, deaths in care homes are 34% of all COVID-19 deaths, whereas deaths of care home residents are 51%.
The data we have gathered so far is summarized in this table, details on all the sources are available in the full report:
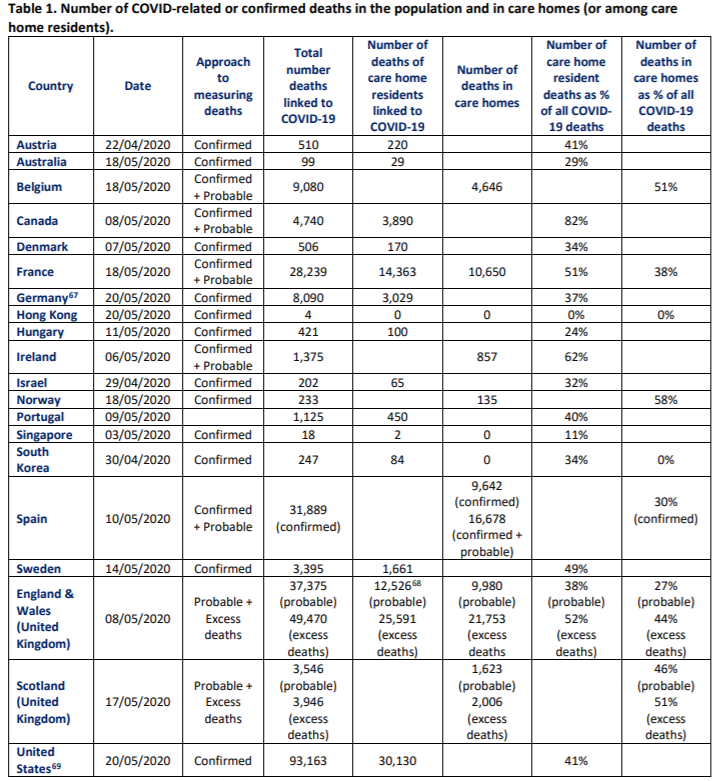
[1] Germany’s definition includes communal establishments such as prisons, so the rate of care home residents may be lower.
[2] This figure is for 1st of May https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/datasets/deathsinvolvingcovid19inthecaresectorenglandandwales, so compared to total COVID-19 deaths on that date (33,365).
[3] Data from 45 states, see country description in the full report.
This report aims to present the data in a way that illustrates these differences. To help improve comparability of data, the authors have developed a form which is included in the report, based on an earlier version piloted in Austria, England, Germany, Scotland and Sweden. We hope that gathering data using this form will improve our understanding of the impact of COVID-10 on people who use or provide long-term care. If you are able to provide data, please email info@ltccovid.org.
As improved comparable data becomes available for more countries, we hope to be able to create graphs that are more comparable too and we may be able to generate datasets that may contribute to improve our understanding of the relationships between different measures adopted to prevent COVID-19 and mortality of care home residents.
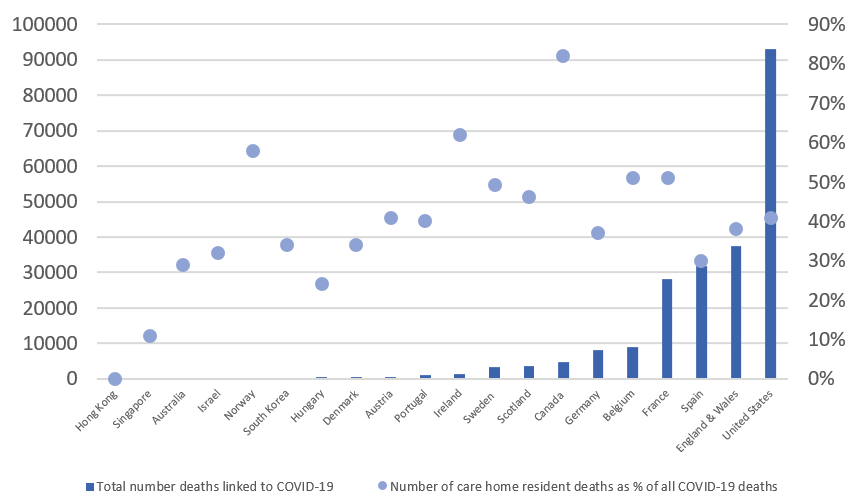
While an early trend observed was that the share of deaths in care homes seemed to increase as the total number of deaths increase, it seems that, at least for the two countries where we have the longest time trends so far (Belgium and France), the share of death becomes relatively stable after a while. In future versions of the report we will seek to include trends for more countries and, where possible, data disaggregated by age and gender.
For a few countries we have been able to estimate the share of all care home residents whose deaths are linked to COVID-19. These range from 0 in Hong Kong, 0.3% in Austria, 0.4% in Germany and 0.9% in Canada, to 2% in Sweden, 2.4% in France and 3.7% in Belgium. In the UK, if only deaths in care homes registered as linked to COVID-19, the figure would be 2.8, whereas if excess deaths of care home residents is used, it would be 6.7% (this does not include deaths of Scottish care home residents in hospitals or deaths in care homes in Northern Ireland, so the share may be a bit higher).
| Number of care home residents (or beds) | Deaths attributed to COVID (as per table 1) as percentage of care home residents | Excess deaths compared to previous years, as percentage of care home residents | |
| Austria | 69,730 | 0.3% | |
| Belgium | 125,000 | 3.7% | |
| Canada | 425,755 | 0.9% | |
| France | 605,061 | 2.4% | |
| Germany | 818,000 (beds) | 0.4% | |
| Sweden | 82,217 | 2.0% | |
| United Kingdom[1] | 411,000 | 3.4% | 6.7% |
[1] The share is likely to be an underestimate as data for deaths in care homes are not available for Northern Ireland and deaths of residents in care homes from Scotland who died in hospital have not been included.
Recognizing the disproportionate impact of COVID-19 on people who live in care homes is an important first step to ensure that efforts to prevent further spread do not leave out the people who are most at risk. A report on international examples of measures to prevent and mitigate the impact of COVID-19 on people who live and work in care homes is available here.
